Toripalimab is licensed for use in the 3rd-line setting in China for recurrent or metastatic (R/M) nasopharyngeal carcinoma (NPC). Presented recently at ASCO 2021, the phase III JUPITER-02 trial, which investigated toripalimab combined with cisplatin and gemcitabine (GP) in the 1st-line setting for R/M NPC, offered results that support this combination at the new standard of care in this setting.
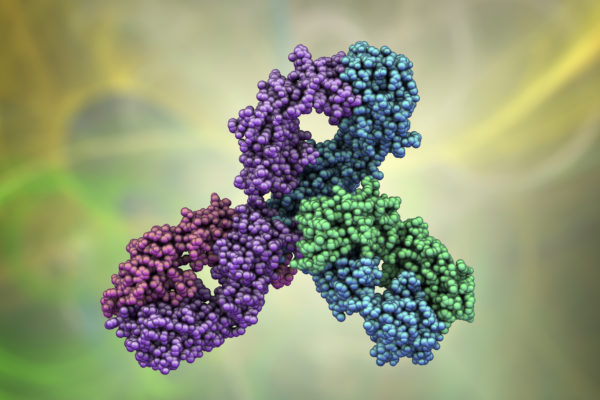
NPC is an endemic malignancy in the Southern China and Southeast Asia regions, with an incidence of 3.0 per 100,000 in China. Comparatively, the global incidence rate is 1.2 per 100,000. Toripalimab, an anti-PD-1 IgG4K monocloncal antibody was found to provide a survival benefit in this setting in the POLARIS-02 trial (median overall survival [mOS]: 17.4 months; median progression-free survival [mPFS]: 1.9 months). Subsequently, toripalimab was approved in the 3rd line setting R/M NPC in China as of February 2021. Investigating toripalimab in the 1st line setting of NPC, in combination with the current global standard of care, GP chemotherapy, the results of the phase III JUPITER-02 trial were recently presented at ASCO 2021.
This double-blind, multicentre study randomised 189 treatment naïve R/M NPC patients (1:1) to receive toripalimab (240mg day 1, every 3 weeks), or placebo, in combination with gemcitabine (1000mg/m2, days 1 and 2 every 3 weeks) and cisplatin (80mg/m2 day 1 every 3 weeks) for up to 6 cycles, followed by toripalimab or placebo monotherapy (every 3 weeks) until disease progression, unacceptable toxicity or completion of 2 years of treatment. The primary endpoint of this study was PFS, with secondary endpoints of objective response rate (ORR), duration of response (DoR), OS and safety.
Baseline characteristics were generally well balanced between the two arms. The median age of patients in this study was 46 in the toripalimab arm, and 51 in the placebo arm. Approximately 83% were male and 75% of patients were found to have PD-L1 positive tumours. 98% of cases were non-keratinising squamous cell carcinoma histology. With an interim analysis data cut-off date of May 30th 2020, a significant improvement in PFS was found with toripalimab when compared to placebo (11.7 months vs. 8.0 months; HR[95%CI]: 0.52[0.36-0.74], P = 0.0003). At one year, the PFS rate was 49% and 28%, respectively. A PFS benefit with toripalimab was observed across al prespecified subgroups, including both PD-L1 positive and negative patients. OS data was not mature, with 25 deaths occurring in the toripalimab arm, and 39 in the placebo arm. In both arms of the study, the mOS was not reached (HR[95%CI]: 0.603[0.364-0.997], P = 0.0462). The one-year OS rate was higher in patients who received toripalimab, at 91.6%, compared to 87.1% in the placebo group. This benefit with toripalimab expanded at 2 years to a survival rate of 78% and 63%, respectively. The ORR was also better with toripalimab at 77.4% vs. 66.4% with placebo (P = 0.033). Crucially, a complete response was observed in 19.2% of patients who received toripalimab, in contrast to 11.2% who received placebo. The mDoR was also extended with toripalimab, at 10.0 months vs. 5.7 months with placebo (HR[95%CI]: 0.50[0.33-0.78], P = 0.0014). The incidence of grade >_3 treatment-emergent adverse events (TEAEs) was similar between toripalimab and placebo arms (89.0% vs. 89.5%). The most common grade >_3 TEAEs included leukopenia (61.6% vs. 58.0%), anaemia (47.3% vs. 39.9%) and neutropenia (57.5% vs. 63.6%). Unsurprisingly, grade >_3 immune-related AEs were higher in patients treated with toripalimab (7.5% vs. 0.7%). AEs leading to discontinuation of toripalimab or placebo occurred in 7.5% and 4.9% of patients, respectively. Fatal AEs were comparable between the two arms (2.7% vs. 2.8%).
Conclusion
The combination of toripalimab to GP in a 1st line setting for R/M NPC significantly improved survival outcomes and resulted in a manageable safety profile. These results support the combination as a new standard of care in this setting.
Thoughts from key opinion leaders
Dr. Nicholas Rohs, an assistant professor of medicine, hematology and medical oncology at The Tisch Cancer Institute at Mount Sinai, in New York City, commented on the trial, saying that “While nasopharyngeal cancer is a fairly chemosensitive disease responses can be brief with decreasing benefit from subsequent therapies leaving significant unmet needs in this space. It’s encouraging to see a >20% increase in 1-year PFS, hopefully indicative of a population of patients who will derive prolonged benefit, as well as PFS benefit across all PDL-1 subgroups. I look forward to seeing more mature data with overall survival results and more granular breakdown of sub-groups, but this is likely ushering in the advent of chemo-IO as standard of care in this setting.”
The study was also discussed at the recent ASCO 2021 meeting, with ASCOs chief medical officer, Dr. Julie Gralow, saying “This is one of the first studies in metastatic or recurrent nasopharyngeal carcinoma to show a benefit of the combination of a PD-1 inhibitor with chemotherapy. Toripalimab is currently approved in China for several indications, including the third-line setting for metastatic nasopharyngeal carcinoma. In the U.S., it’s received breakthrough-therapy designation by the U.S. FDA (Food and Drug Administration) for recurrent metastatic nasopharyngeal carcinoma, as well as fast-track and orphan drug status for other cancer types. With FDA approval, these findings should prove to be practice changing.”